GENERAL MEDICINE
17/10/2023 60 year male with diminution of vision since 4 months .
Hi, I am Pindi Gayatri, 5th sem medical student. This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CONSENT AND DE-IDENTIFICATION :
The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed throughout this piece of work whatsoever.
Chief Complaint:
60 year old male farmer by occupation resident of suryapet came to OPD with chief complaints of
-diminution of vision of both eyes since 4 months
History of Present Illness:
Patient was apparently asymptomatic 4 months ago then he developed diminution of vision in both the eyes which is insidious in onset and gradually progressive.
Known case of Asthma since 10 years ,on inhalers on and off . Last used 3 days back.
History of pulmonary TB 40 years ago used ATT(Details unknown).
C/o breathlessness grade 1 MMRC+ not associated with wheeze . Aggravated on exertion.
No h/o any itching of eye,redness,watering,trauma.
No h/o of fever,chest pain, chest tightness,hemoptysis,palpitations, SOB, orthopnea, PND,Pedal edema, decreased urine output.
No h/o loss of weight and appetite.
Past History:
Not a k/c/o DM,HTN,Thyroid disorders, CAD,CVA, TB, epilepsy.
Personal History:
- married
-appetite normal
- mixed diet
-sleep adequate
- regular bowels and bladder
- normal micturition
- no known allergies
- No addictions
Family History: not significant
Drug History:
On Ipratropium bromide and levosalbutamol sulphate rotacap inhalers -for asthma since 10 years.
General Examination:
I have examined the patient after taken prior consent and informing the patient in the presence of a female attendant. The examination was done in both supine and sitting position in a well lit room.
- patient was conscious, coherent and cooperative
- well oriented to time, place and person.
- well built and moderately nourished
- no pallor
- no icterus
- no cyanosis
- no clubbing of fingers
- no lymphadenopathy
- no edema of feet
- no malnutrition
- no dehydration
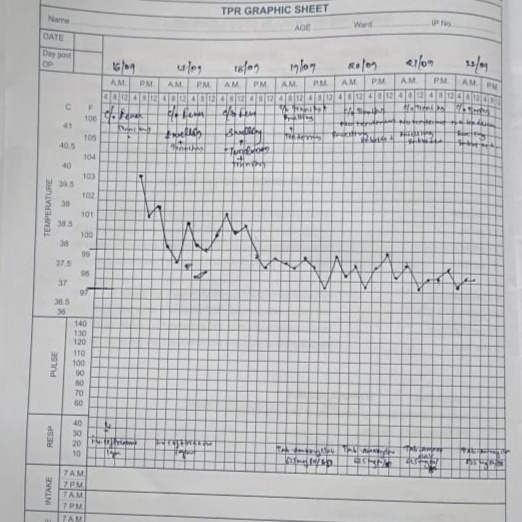
Vitals:
- Temperature: afebrile
-BP:150/90 mm Hg
-Pulse:76 beats/min
- RR:16 cycles/min
Systemic Examination:
CVS
No thrills
S1S2 sounds heard
No cardiac murmurs
RESPIRATORY SYSTEM
- upper respiratory tract : oral cavity, nose & oropharynx appear normal
- chest is bilaterally symmetrical
- respiratory movements appear equal on both sides and of thoracoabdominal type
Position of trachea-central
Vesicular breath sounds heard
No dyspnea
Wheeze +in bilateral ISA,IAA.
ABDOMEN
Shape of the abdomen-scaphoid
No tenderness
No palpable masses
Normal hernial orifices
No free fluid
No bruits
Non palpable liver
Non Palpable spleen
No Bowel sounds heard
CNS
Level of consciousness- conscious
Speech- normal
Signs of meningeal irritation
stiffness of neck :no
Kerning's sign:no
Cranial nerves,motor system, sensory system-normal
Reflexes
Biceps Triceps supinator knee ankle
Right 2+ 2+ 2+ 2+ 2+
Left 2+ 2+ 2+ 2+ 2+
Cerebellar signs:
- finger nose in coordination: not seen
- knee heel in coordination: not seen
Investigations:
Hemogram:
Hb:13.0
TLC:10,700
N/L/E/M: 73/14/3/10
PLT:3.26
RFT:
BU:20
SC:0.8
Na+:135
K+:4.5
Cl-:103
LFT:
TB:0.64
PB:0.19
SGOT:122
SGPT:138
ALP:291
TP:6.8
Alb:4.2
A/G:1.66
2D ECHO :
EF:6.3
Concentric LVH,No RWMA
IVC:1.12 cm collapsing
RVSP:35 mm Hg
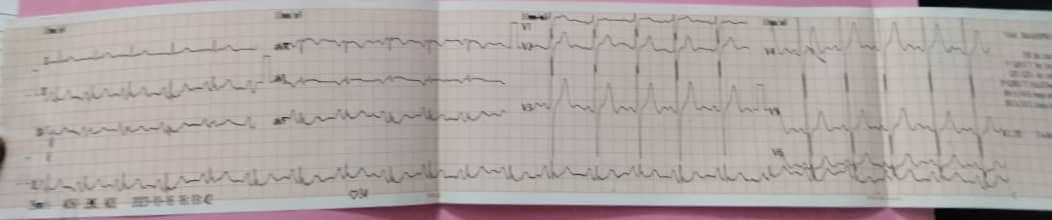
ECG:
Negative
CXR PA view:
Right unilateral fibrosis
RS:
BAE+,VBS+,
BL Rhonchi +,inter SA,Infra SA,
IAA,AA,ICA,MA.
Provisional Diagnosis:
*Left eye -senile mature cataract associated with denovo hypertension
*Known case of bronchial asthma since 10 years ,on medication.
*Asthma/COPD?(PFTB).
Medication:
E/D ciplox-2°-eye-QID
Tab Nicardia-oral