GENERAL MEDICINE
55 year male with SOB,dry cough, decreased urinary output
September 24, 2023
Hi, I am Pindi Gayatri, 5th sem medical student. This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CONSENT AND DE-IDENTIFICATION :
The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed throughout this piece of work whatever.
Chief Complaint:
-A 55yr old male patient resident of haliya came to general medicine opd with cheif complaints of SOB since 1week,dry cough since 3days,decreased urine output since 15days.
History of Present Illness:
-Patient was apparently aymptomatic 6months back. Then he was on hemodialysis from6mnths back from june 2023.
-Then he developed shortness of breath since 1week which is of grade 4 and insidious in onset and gradually progressive in nature which is aggrevated on talking and relieved on taking rest.
-There is ARI with dry cough since 3days.
-Bilateral pedal edema which is of pitting type is seen.
-Decreased urine output since 15 days is seen.
Daily Routine:
Before he got sick, he used to wake up at 5am every morning, take a bath at 6.30am, eat breakfast of rice and curry and leave for work by 8.30am. He is a daily wage laborer by occupation and he used to pack lunch which was the same rice and curry as breakfast and eat it at her workplace. He used to reach home by 7 or 8pm after which he eat and sleep by 11pm.
After he got sick, he stopped going to work and stayed at home, following which he was admitted into the hospital.
Past History:
- No similar complaints
-He is a k/c/o HTN sicne 6months
-K/c/o DM since 20days
-Is a k/c/o CKD since 2 and half yrs
-Is k/c/o hypothyroidism from 1month.
-Not a k/c/o CAD,CVA,asthma, epilepsy.
Surgical history: no surgical history
Personal History:
- married
- decreased appetite
- mixed diet
- Sleep adequate
- regular bowels
- abnormal micturition
- no known allergies
- addictions: occasionally drinks alcohol, 4-5 beedis per day
Family History: not significant
General Examination:
I have examined the patient after taken prior consent and informing the patient in the presence of a female attendant. The examination was done in both supine and sitting position in a well lit room.
- patient was conscious, coherent and cooperative
- well oriented to time and space
- well built and adequately nourished
- no pallor
- no icterus
- no cyanosis
- no clubbing of fingers
- no lymphadenopathy
- edema of feet present
- no malnutrition
- no dehydration
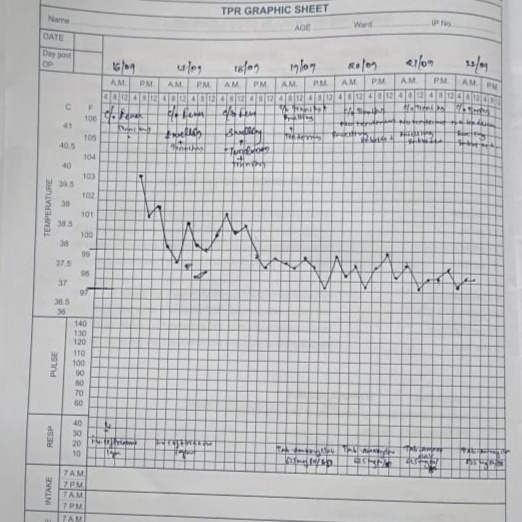
Vitals:
- Temperature: afebrile
- Pulse: 82 beats/min
- RR: 16 cycles/min
- BP: 140/80 mm Hg measured in right arm in supine position
Systemic Examination:
Respiratory System
- upper respiratory tract : oral cavity, nose & oropharynx appear normal
- chest is bilaterally symmetrical
- respiratory movements appear equal on both sides and of thoracoabdominal type
- position of trachea : central
- vesicular breath sounds : present
- no wheeze
Cardiovascular System:
Inspection :
- shape of chest : elliptical
- no engorged veins, scars, visible pulsations
Palpation :
-Apex beat can be palpable in 5th intercostal space
- no cardiac thrills
Auscultation :
- S1,S2 are heard
- no murmurs
Abdomen:
- shape: obese
- no tenderness
- no palpable mass
- no bruits
- no free fluid
- hernias orifices: normal
- liver: not palpable
- spleen : not palpable
- no bowel sounds
- genitals: normal
- speculum examination : normal
- P/R examination : normal
Central Nervous System:
- conscious
- normal speech
- no neck stiffness
- no Kerning's sign
- cranial nerves: normal
- sensory : normal
- motor: normal
- reflexes: all present bilaterally
- finger nose in coordination: not seen
- knee heel in coordination: not seen
- gait: normal
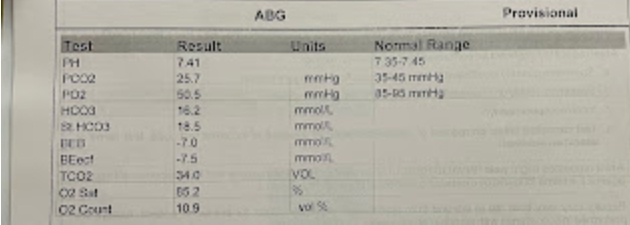
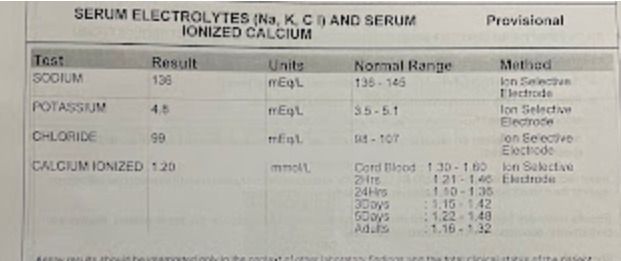
Provisional Diagnosis:
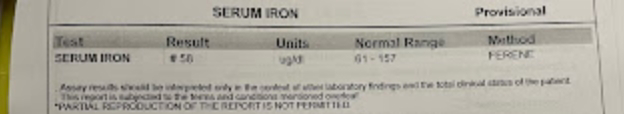
-CKD on MHD with k/c/o Hypertension and DM
-K/c/o Hypothyroidism
Treatment:
1.Fluid restriction <5L per day
2.Salt restriction <2gms per day
3.T.lasix 20mg po/bd
4.Inj PAN IV /OD
5.Inj ZOFER IV/OD
6.Tab AMLONG 10mg po/bd
7.T NODOSIS 500mg po/bd
8. OROFER po/bd
9. INJ NEOMOL 1g IV
10. T DOLO 650 po/bd
11. INJ ERYTHROPOIETIN IV s/c twice weekly
12. Monitor vitals 4th hourly
13. Inform SOS